Revenue Cycle Management (RCM) plays a critical role in the healthcare industry. It encompasses the entire financial process of healthcare services, from the moment a patient makes an appointment to when the payment is collected. Given the complexities of insurance claims, medical billing and coding, effective RCM can make the difference between a financially successful healthcare practice and one that struggles to maintain profitability.
Here we discuss revenue cycle management, its significance in healthcare, and the best practices healthcare providers should implement to ensure smooth operations. Additionally, we’ll dive into the role of revenue codes in the RCM process, identify common errors, and offer some insights into optimizing the revenue cycle with RCM in healthcare.
What is Revenue Cycle Management in Healthcare?
Revenue cycle management (RCM) refers to the process that healthcare BPO companies use to manage the financial aspects of patient care. This process involves all administrative and clinical functions that contribute to capturing, managing, and collecting patient revenue. The cycle starts when a patient makes an appointment and ends when the healthcare provider receives full payment for services rendered.
An effective healthcare revenue cycle management system ensures that healthcare providers receive appropriate and timely reimbursement for the services they provide, which is essential for the financial health of the practice.
The Importance of Revenue Cycle Management in Healthcare
The importance of revenue cycle management in healthcare cannot be overstated. Efficient RCM services helps healthcare providers:
Maximize Revenue
By streamlining billing and coding processes, healthcare providers can capture more revenue and reduce the risk of missing out on payments due to errors or inefficiencies.
Improve Cash Flow
By managing claims, denials, and collections in a timely manner, RCM ensures that cash flow remains steady, allowing the practice to cover operational expenses and reinvest in growth.
Reduce Errors and Denials
Effective RCM minimizes the chances of submitting incorrect claims that lead to costly denials. When claims are denied, they must be corrected and resubmitted, which takes up valuable time and resources.
Ensure Compliance
With ever-changing regulations, especially from entities like CMS (Centers for Medicare & Medicaid Services), staying compliant is a significant part of RCM in healthcare. An efficient RCM system ensures that all coding and billing practices comply with current standards.
Enhance Patient Experience
By simplifying billing and communication processes, RCM helps avoid confusion and frustration on the part of patients, making the overall experience smoother and more transparent.
Also Read: Accounts Receivable in RCM: Benefits and Importance
The Revenue Cycle: A Step-by-Step Process
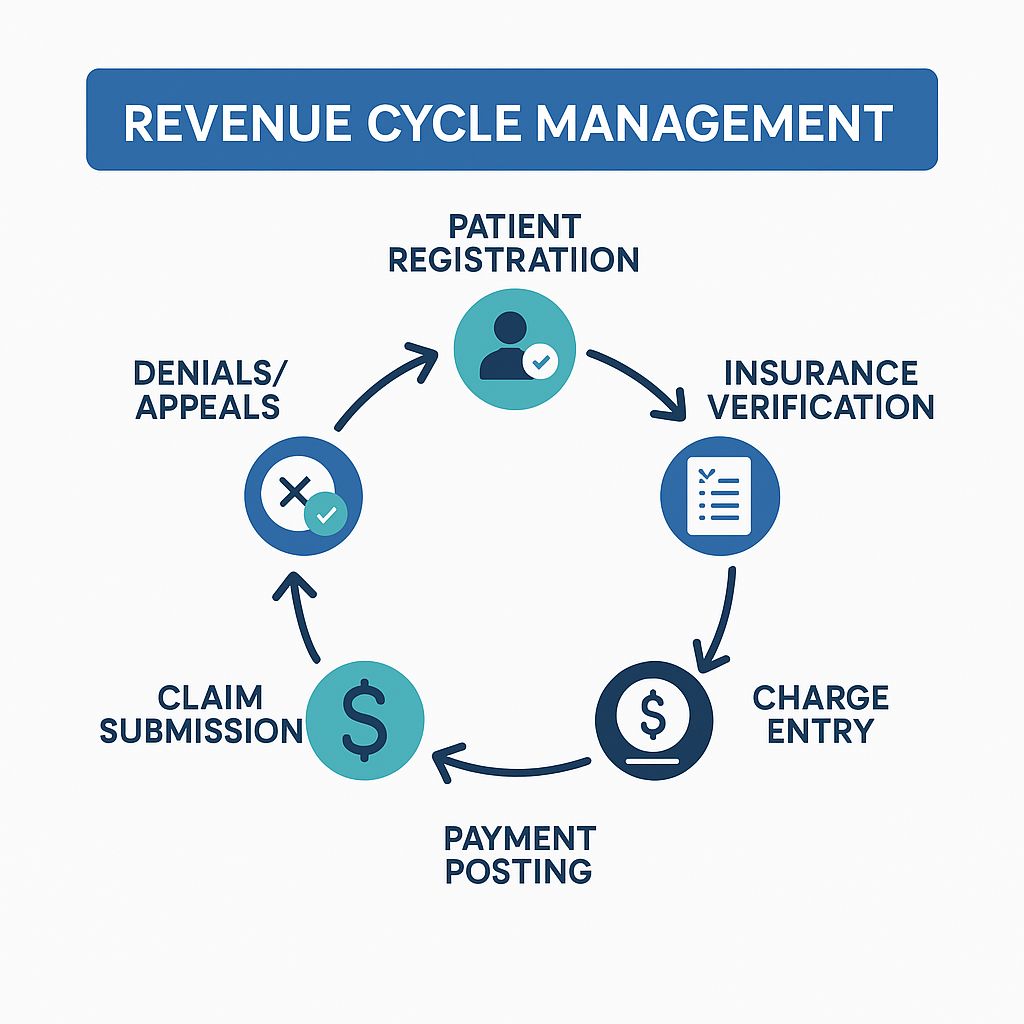
Pre-Registration
This is the first step where patient information is collected, including demographics, insurance details, and the nature of their visit. Accurate data collection here is essential for billing accuracy.
Insurance Verification
Before treatment, the patient’s insurance coverage is verified. This step ensures that the patient’s insurance will cover the required services and helps to avoid unexpected denials.
Charge Capture
This process involves documenting the services provided, including procedures, consultations, and any medical supplies used during treatment. Charge capture must be accurate to ensure that all services are billed correctly.
Coding
Once the services are documented, the medical coding process begins. Healthcare providers and medical coders use specific codes (CPT, ICD-10, HCPCS) to describe the diagnosis, procedures, and services provided. Accurate coding is crucial for ensuring correct reimbursement and avoiding denials.
Claim Submission
After coding, the claim is submitted to the insurance company. Timely and accurate submission is essential for reducing the chances of delayed payments or denials.
Payment Posting
Once the insurance company processes the claim, payments are posted, and any remaining balance is sent to the patient. This step also involves reconciling any differences between the expected and actual payments. So you need expert payment posting services.
Denial Management
When claims are denied or underpaid, it is essential to analyze the reasons for the denial and correct any errors. Denial management is a critical aspect of maintaining cash flow and profitability in healthcare organizations.
Patient Collections
Finally, any outstanding balances from the patient are collected. This step involves clear communication about the amount due and the payment options available to the patient.
The Role of Revenue Codes in the Revenue Cycle
Revenue codes are essential components of revenue cycle management in the healthcare process. These codes are used to describe the specific services or treatments provided to patients. They play a critical role in the billing process and are used to link specific procedures or services to appropriate payment amounts.
For example, if a patient undergoes a particular diagnostic test, the revenue code will help ensure that the claim reflects the correct service, which impacts reimbursement. Accurate revenue coding is crucial because errors can lead to underpayment or claim rejection, which ultimately affects the practice’s revenue.
Common Revenue Code Errors and How to Avoid Them
Incorrect Coding
One of the most common errors in the revenue cycle is incorrect coding, such as using outdated codes or misidentifying a service. This can lead to claim denials and delayed payments. So you need an expert who is the best in BPO operations.
Best Practice
Keep up to date with coding guidelines, including regular training for your coding team. Regular audits are also recommended to identify and correct errors.
Missing Revenue Codes
Failing to include the correct revenue code for a procedure or service can result in the insurance provider not reimbursing the claim.
Best Practice
Ensure that the revenue codes align with the CPT and ICD codes used. Utilize coding software that can automatically assign revenue codes based on the procedure.
Incorrect Modifiers
Sometimes, claims are submitted with incorrect or missing modifiers, which indicate specific details about a service, such as whether a procedure was bilateral or performed in an outpatient setting.
Best Practice
Double-check modifiers before submission. Ensure that modifiers are only applied when necessary and that they are used correctly.
Best Practices for Optimizing Revenue Cycle Management in Healthcare
Automate Processes
Automation tools can help streamline many aspects of RCM, including billing, coding, and claims submission. This can reduce human error and increase operational efficiency.
Train Staff Regularly
Continuous education and training for your team on billing, coding, and RCM best practices are essential for maintaining accuracy and compliance.
Leverage Analytics
Use data analytics to track key performance indicators (KPIs) in the revenue cycle. This will allow healthcare organizations to identify inefficiencies, such as prolonged denials or delays in payments, and take corrective action.
Implement Robust Denial Management
Denial management should be a proactive part of the RCM process. By promptly addressing denials and identifying trends, healthcare providers can reduce the overall impact on revenue.
Maintain Clear Communication with Patients
Transparency in billing practices is essential for patient satisfaction. Ensure that patients understand their financial responsibility upfront and offer clear payment options.
Compliance in Revenue Cycle Management
Adhering to regulatory standards is a crucial aspect of revenue cycle management in healthcare. Compliance with codes, insurance regulations, and healthcare laws is mandatory. Healthcare providers must stay updated on the latest guidelines from regulatory bodies like CMS (Centers for Medicare & Medicaid Services) and the AMA (American Medical Association).
Regular compliance checks and audits should be performed to ensure that all processes comply with the most current regulations and that all billing practices are aligned with industry standards. A failure to comply with regulations can result in fines, penalties, or audits.
How AffinityCore Can Help
At AffinityCore, we specialize in revenue cycle management services for healthcare providers. Our team of experts helps practices navigate the complexities of billing, coding, and insurance claims, ensuring that your practice is compliant, efficient, and financially sound.
By outsourcing your RCM to us, you can take BPO benefits. So you can focus on delivering quality care while we handle the revenue cycle behind the scenes. We offer tailored solutions that reduce denials, improve cash flow, and ensure that you are reimbursed promptly for your services.
Conclusion
Effective revenue cycle management is essential for the success of healthcare organizations. From pre-registration to patient collections, every step of the cycle plays a significant role in ensuring that healthcare providers receive appropriate payment for their services. By understanding the importance of RCM and implementing best practices, healthcare providers can maximize revenue, improve cash flow, and enhance the patient’s experience.
At AffinityCore, we are committed to helping healthcare providers optimize their RCM in the healthcare process. Our team is here to support your practice with streamlined billing, coding, and revenue cycle management services, ensuring that you can focus on what matters most: providing excellent patient care.
FAQS
Q1.What is the RCM process workflow?
Ans: The Revenue Cycle Management (RCM) process workflow includes patient registration, insurance verification, medical coding, charge entry, claim submission, payment posting, and handling denials or appeals. It ensures healthcare providers receive accurate and timely reimbursement for services delivered.
Q2.What are the 4 steps in the Revenue Cycle?
Ans: The four main steps in the revenue cycle are:
-
Patient Registration: Collecting patient and insurance details.
-
Charge Capture: Recording services provided.
-
Claim Submission: Sending claims to payers.
-
Payment Posting: Applying payments and handling any follow-ups.
Q3.What are the 4 P’s of revenue cycle management?
Ans: The 4 P’s of revenue cycle management are Patient, Provider, Payer, and Process. Each plays a vital role in RCM efficiency.
Q4.How Can Affinitycore Help in Revenue Cycle Management?
Ans: AffinityCore supports healthcare Revenue Cycle Management by handling medical billing, coding, claims processing, and payment posting with accuracy and compliance. Their services help providers reduce denials, speed up reimbursements, and improve overall financial performance.

